Frequently Asked Questions: Biocompatibility & FDA Certification Standards for Dental 3D Printing Resin
General Questions about FDA Clearance
Q1: What’s the difference between a “biocompatible” resin and an “FDA-cleared” resin?
A: These terms represent fundamentally different levels of regulatory validation and are often confused in marketing materials.
Biocompatible Resin is a general marketing claim that suggests a material has undergone some level of biocompatibility testing, but biocompatibility claims can be based on limited testing, different applications than intended, or third-party studies with unclear relevance. A resin might be biocompatible for one application but inappropriate for another. Without FDA regulatory oversight, biocompatibility claims lack standardized enforcement or verification.
FDA-Cleared Resin has completed the FDA 510(k) premarket notification process, demonstrating substantial equivalence to an already-cleared predicate device. This clearance is specific to an intended use—for example, LuxCreo’s DCA (Dental Clear Aligner) resin is FDA Class II 510(k) cleared specifically for direct-print clear aligners contacting oral mucosa for extended periods. The manufacturer must submit comprehensive biocompatibility testing, manufacturing quality controls, and clinical data. The FDA evaluates all evidence and issues written clearance.
The practical difference: FDA-cleared resins carry regulatory validation that manufacturers have met rigorous standards for specific clinical applications. Biocompatible claims alone do not guarantee regulatory approval or suitability for patient contact.
Q2: What does “FDA Class I” versus “FDA Class II” mean for dental resins?
A: FDA classification reflects the regulatory risk level associated with the device’s intended use and tissue contact characteristics.
FDA Class I Resins represent the lowest regulatory risk category. These materials are intended for applications with minimal biological interaction—diagnostic models used for treatment planning (but not inserted in the mouth), surgical guides that will be sterilized and discarded, or components that undergo further processing into other products. Class I resins may not require premarket notification (510(k)) clearance, though manufacturers must comply with quality system (QSR) and good manufacturing practices (GMP).
LuxCreo’s DSG (Dental Surgical Guide) resin exemplifies Class I certification. This material is FDA Class I certified because surgical guides are used for implant planning and then removed—they don’t remain in the mouth.
FDA Class II Resins carry higher regulatory requirements because they are intended for direct or prolonged intraoral contact. Clear aligners worn 22 hours daily, night guards, splints, crowns, denture bases, and temporary restorations all fall into Class II because they contact oral tissues for extended periods. Manufacturers must submit FDA 510(k) premarket notification demonstrating substantial equivalence to an established predicate device, plus comprehensive biocompatibility testing.
LuxCreo’s DCA resin received FDA Class II 510(k) clearance—a historic achievement because it was the first direct-print clear aligner resin to achieve this classification. This clearance enables orthodontists and labs to legally print aligners directly without thermoforming.
Regulatory pathway difference: Class I requires documentation but not premarket approval. Class II requires FDA 510(k) submission, review, and clearance before marketing.
Q3: How long does FDA 510(k) clearance take?
A: The FDA’s target review time for 510(k) submissions is 90 days from submission to clearance decision. However, several factors can extend this timeline:
- Substantial Equivalence Assessment: If the FDA cannot clearly establish substantial equivalence to a predicate device, they issue a “Complete Deficiency Notice” requesting additional information.
- Additional Testing Requirements: The FDA may request additional biocompatibility data, mechanical property testing, or clinical evidence before clearing the submission.
- Predicate Device Identification: Choosing an appropriate predicate device—a legally marketed comparable resin with similar properties and intended use—is critical. Weak predicate selection can delay clearance.
LuxCreo’s FDA 510(k) clearance for DCA resin required extensive biocompatibility documentation and demonstration of equivalence to thermoformed aligner materials. First-of-kind devices (like the world’s first direct-print aligner resin) may experience longer review because the FDA lacks direct precedent.
Best practice: Plan for 4–6 months from submission to clearance when preparing regulatory timelines, accounting for potential deficiency notices.
Questions about ISO 10993 Biocompatibility Testing
Q4: What exactly is ISO 10993, and why is it so important for dental resins?
A: ISO 10993 is the International Organization for Standardization (ISO) series of standards that defines how biocompatibility of medical devices—including dental resins—must be tested. It’s the globally recognized framework referenced by the FDA, European Union Medical Device Regulation (MDR), Japan’s PMDA, and China’s NMPA.
ISO 10993 operates on a fundamental principle: biocompatibility assessment must be proportional to the device’s tissue contact characteristics. The standard asks four critical questions:
- Does the device contact tissue? If no tissue contact, biocompatibility testing may not be required.
- What type of contact? External skin, oral mucosa, blood, implantation?
- How long is the contact? Temporary (<24 hours), short-term (24 hours to 30 days), or long-term (>30 days)?
- What is the contact area? Localized or widespread tissue exposure?
For clear aligner resins contacting oral mucosa for weeks, the answer triggers comprehensive testing requirements. Why it matters: This standardized approach ensures manufacturers don’t under-test materials, preventing inadequately validated devices from reaching patients.
Q5: What testing components are included in ISO 10993 biocompatibility evaluation?
A: ISO 10993 comprises multiple parts, each addressing specific biocompatibility endpoints. For long-term intraoral resin devices like aligners, the typical required battery includes:
ISO 10993-5: Cytotoxicity Testing Tests whether the material or its eluted compounds cause cell death, growth inhibition, or reduced cell viability. Three methodology options exist: elution (soaking resin in culture medium, then exposing cells), direct contact (cells touching material), and agar diffusion (material on bacterial plates). Cytotoxicity testing is the foundation—if a material is cytotoxic, it’s contraindicated for intraoral use.
Research shows post-processing dramatically impacts cytotoxicity. Studies comparing fresh versus processed dental resin samples demonstrate that ethanol washing can markedly decrease material toxicity, making standardized cleaning protocols essential for compliance.
ISO 10993-10: Sensitization and Irritation Testing
Evaluates whether a material triggers allergic reactions (sensitization) or acute inflammatory responses (irritation). Tests use animal models to assess delayed-type hypersensitivity following repeated exposure. For aligners maintaining direct mucosal contact, sensitization testing is critical because residual monomers can accumulate and trigger allergic reactions in susceptible patients.
ISO 10993-11: Systemic Toxicity Testing
Determines whether absorbed or metabolized compounds cause generalized biological effects—organ damage, reproductive toxicity, or systemic inflammation. Testing includes acute systemic toxicity (single exposure), subacute/subchronic toxicity (repeated doses over days or weeks), and chronic toxicity (extended exposure).
ISO 10993-3: Genotoxicity Testing Evaluates whether compounds from the material cause genetic damage (mutations or chromosomal alterations) that could increase cancer risk. Standard tests include Ames bacterial mutagenesis, mammalian cell mutations, and chromosomal aberration assays. This testing is particularly important for resins with uncrosslinked monomers that could leach into saliva.
LuxCreo’s DCA resin exemplifies comprehensive testing. This material underwent the complete ISO 10993 battery—cytotoxicity, oral mucosal irritation, skin sensitization, genotoxicity, acute/subchronic systemic toxicity, subcutaneous implantation, and pyrogenic response testing—demonstrating commitment to patient safety beyond minimum FDA requirements.
Q6: Why does post-processing (washing and curing) matter for biocompatibility?
A: Post-processing fundamentally influences material biocompatibility because many dental resins contain residual uncrosslinked monomers or reactive oligomers that can leach into saliva, potentially causing tissue irritation, sensitization, or systemic effects.
ISO 10993-5 cytotoxicity testing accounts for this reality by testing materials in two states:
- Freshly prepared material: Captures maximum monomer concentration immediately after printing
- Processed material: Tests the resin after manufacturer-recommended washing and curing, reflecting clinical reality
Validated washing protocols substantially reduce cytotoxicity. Research comparing brief versus extended isopropyl alcohol (IPA) washing demonstrates that increased washing duration—particularly with ultrasonic agitation—effectively removes unreacted monomers, improving biocompatibility profiles.
For example, LuxCreo’s DCA aligner workflow specifies:
- Washing: Two 8-minute ultrasonic cycles in IPA solution
- Heat curing: 10 minutes (if printed with DCA)
- UV curing: 10 minutes per side under 405 nm light to achieve full mechanical properties and biocompatibility
Critical implication: Skipping or modifying manufacturer-recommended washing and curing steps fundamentally alters the material’s tested biocompatibility characteristics. Clinical teams must strictly adhere to validated protocols to ensure compliance with FDA clearance and ISO 10993 testing evidence.
Questions about Specific FDA-Cleared Dental Resins
Q7: Which dental 3D printing resins currently have FDA clearance?
A: Several manufacturers have achieved FDA 510(k) clearance for specific applications. Here are the primary FDA-cleared options:
LuxCreo DCA (Dental Clear Aligner) Resin
- FDA Classification: Class II 510(k) cleared
- International Approvals: CE IIA (Europe), NMPA Class II (China), PMDA (Japan), TFDA (Taiwan), Canada Class II
- Intended Use: Direct-print clear aligners for orthodontic treatment
- Unique Feature: World’s first FDA Class II 510(k) cleared direct-print aligner resin, featuring ActiveMemory™ shape memory technology
- Biocompatibility: Complete ISO 10993 testing including cytotoxicity, oral irritation, sensitization, genotoxicity, systemic toxicity, subcutaneous implantation
LuxCreo DSG (Dental Surgical Guide) Resin
- FDA Classification: Class I certified
- Intended Use: Orthodontic surgical guides for implant planning
- Biocompatibility: ISO 10993-5 (cytotoxicity), ISO 10993-10 (sensitization/irritation)
Formlabs Premium Teeth Resin
- FDA Classification: Class II 510(k) cleared (August 2024)
- Intended Use: Temporary crowns, inlays, onlays, veneers, and temporary bridges (up to seven units)
- Material: Nano-ceramic-filled biocompatible composite
Formlabs BEGO™ VarseoSmile® TriniQ® Resin
- FDA Classification: Class II 510(k) cleared
- Intended Use: Permanent single-unit crowns, inlays, onlays, veneers; permanent bridges (up to three units); denture teeth
- Unique Feature: First 3D printing resin indicated for permanent bridges
SprintRay Ceramic Crown C2
- FDA Classification: Class II 510(k) cleared
- Intended Use: Definitive individual and fixed full single crowns, partial crowns, individual veneers, artificial teeth for dentures
- Material: Ceramic-filled composite
Desktop Health Flexcera Smile Ultra+
- FDA Classification: Class II 510(k) cleared
- International Approvals: CE MDR Class IIa, multiple international certifications
- Intended Use: Temporary and permanent restoration applications
3D Systems NextDent Jetted Denture Solution
- FDA Classification: Class II 510(k) cleared (2025)
- Intended Use: Complete monolithic dentures
- Technology: Multi-Jet 3D printing with minimal post-processing
Note: This list represents major FDA-cleared products as of January 2026. The regulatory landscape continues evolving as manufacturers pursue clearance for new indications.
Q8: What does it mean that LuxCreo’s DCA resin is “FDA Class II 510(k) cleared” specifically for direct-print aligners?
A: This clearance is historically significant and represents a fundamental validation of 3D-printed aligner technology. Here’s what it means:
Predicate Equivalence: LuxCreo demonstrated substantial equivalence to thermoformed aligner materials—the established standard-of-care. The FDA accepted that DCA resin performs equivalently for the intended use (orthodontic alignment therapy) despite being manufactured differently (direct 3D printing vs. thermoforming).
Comprehensive Biocompatibility Evidence: The submission included complete ISO 10993 testing demonstrating the material is safe for 22+ hour daily intraoral contact. This evidence proved DCA resin doesn’t cause cytotoxicity, sensitization, irritation, or systemic effects at levels that would preclude patient use.
ActiveMemory™ Technology Validation: DCA’s shape memory properties—where aligners recover original geometry and force delivery upon heat activation—underwent specific testing to ensure the shape memory cycling doesn’t compromise material safety or biocompatibility.
Clinical Pathway Enablement: This clearance legally authorizes practitioners to print aligners directly without thermoforming, enabling same-day delivery models impossible with traditional workflows.
Competitive Distinction: No other direct-print aligner resin currently holds this FDA Class II 510(k) clearance, giving LuxCreo a regulatory advantage that competitors cannot match until they pursue and obtain their own clearances.
Q9: Can I use non-FDA-cleared resins for dental applications if they claim to be biocompatible?
A: Using non-FDA-cleared resins for intraoral patient contact applications creates significant clinical, legal, and regulatory risks that practitioners should understand carefully.
Regulatory Risk:
- Products lacking FDA 510(k) clearance for specific applications are not legally cleared for that use, even if biocompatible claims exist
- Using non-cleared devices in clinical practice without proper regulatory status may violate FDA enforcement policy
- Practitioners bear liability if patients suffer adverse effects from unvalidated materials
Clinical Uncertainty:
- Biocompatible claims without FDA clearance are not standardized or regulated—manufacturers can make assertions without third-party verification
- A resin might be safely tested for one application but inappropriate for another (e.g., safe for temporary restorations but unsafe for long-term aligners)
- Post-processing protocols may not have been validated, meaning actual clinical materials may differ significantly from tested formulations
Quality Variation:
- Non-FDA-cleared resins may lack ISO 13485 quality management system certification, meaning batch-to-batch variation, contamination, or consistency issues could occur
- Manufacturing changes could alter biocompatibility without manufacturer notification
Best Practice: Restrict Dental 3D Printing Resin selection to FDA-cleared products with specific clearance for your intended application. LuxCreo’s DCA for aligners, Formlabs Premium Teeth for restorations, and 3D Systems NextDent for dentures exemplify materials with regulatory validation enabling confident clinical implementation.
International Regulatory Questions
Q10: What’s the difference between FDA clearance, CE marking, and other international certifications?
A: Regulatory approval varies significantly by region, requiring manufacturers to navigate distinct pathways for global commercialization:
FDA (USA) – 510(k) Clearance
- Pathway: 510(k) premarket notification demonstrating substantial equivalence to a predicate device
- Biocompatibility Standard: ISO 10993 (FDA-recognized international standard)
- Timeline: ~90 days for review (target; actual can extend 6+ months with deficiencies)
- Requirement: Specific FDA clearance needed for each intended use
- Regulatory Body: FDA’s Center for Devices and Radiological Health (CDRH)
LuxCreo’s DCA resin obtained FDA Class II 510(k) clearance in 2022, establishing the pathway for direct-print aligner validation.
CE Marking (EU/EEA) – Medical Device Regulation (MDR)
- Pathway: Notified Body review (for Class IIa/IIb devices); includes design dossier, manufacturing quality systems, biocompatibility testing, clinical evidence
- Biocompatibility Standard: ISO 10993; often more stringent interpretation than FDA
- Timeline: 6–12 months typical; more demanding than FDA 510(k)
- Requirement: CE IIA/IIb classification; separate notified body submission
- Key Difference: MDR requires post-market surveillance plans, clinical data, and broader evidence scope
LuxCreo’s DCA resin achieved CE IIA (European equivalent to FDA Class II) certification, indicating manufacturers pursued MDR compliance simultaneously with FDA clearance.
PMDA (Japan) – Regulatory Approval
- Pathway: Submission to Pharmaceuticals and Medical Devices Agency; often requires extensive biocompatibility testing exceeding FDA standards
- Timeline: 6–18 months
- Requirement: Separate approval needed; not equivalent to FDA/CE clearance
NMPA (China) – Device Classification
- Pathway: Registration with National Medical Products Administration; Class I–III classification system
- Timeline: 4–12 months depending on classification
- Requirement: Increasingly rigorous biocompatibility evaluation for Class II/III
Strategic Insight: Manufacturers pursuing global markets typically prioritize MDR compliance first because European standards are stringent. Meeting MDR requirements often facilitates subsequent FDA and international approvals because the evidence exceeds FDA minimum thresholds.
Q11: If a resin has CE marking, does that automatically mean it’s FDA approved?
A: No. CE marking and FDA clearance are distinct regulatory approvals. A product can have CE marking without FDA clearance, and vice versa. Here’s why:
Separate Regulatory Systems:
- FDA (USA) and European Notified Bodies (EU) apply different standards, evidence requirements, and risk assessments
- A material might satisfy European biocompatibility interpretation (ISO 10993) but not FDA predicate equivalence requirements
- Each region requires independent submission and approval
Different Predicate Requirements:
- FDA 510(k) requires demonstration of substantial equivalence to a specific FDA-cleared predicate device
- EU MDR does not require predicate equivalence; it requires conformity with EU requirements
- A resin with EU predicate approval might lack an appropriate FDA predicate
Timeline and Market Entry Implications:
- Many manufacturers pursue MDR clearance first (more comprehensive) then use MDR evidence to support FDA 510(k) submissions
- Some manufacturers obtain CE marking but choose not to pursue FDA clearance due to business strategy or market priorities
Practical Example: Desktop Health’s Flexcera materials achieved both FDA 510(k) clearance and CE MDR Class IIa certification—but these required separate submissions with distinct evidence packages. Neither automatically validated the other; each was independently required.
Best Practice: Verify FDA 510(k) clearance specifically for your intended clinical application. Don’t assume CE marking implies FDA approval.
Practitioner Implementation Questions
Q12: How do I verify that a resin actually has FDA clearance?
A: The FDA maintains a searchable database of 510(k) clearances. Here’s how to verify:
FDA 510(k) Database Search:
- Visit: https://www.accessdata.fda.gov/cdrh_docs/pdf (FDA’s 510(k) document repository)
- Search by:
- Manufacturer name (e.g., “LuxCreo”)
- Material name (e.g., “DCA Resin” or “Dental Clear Aligner”)
- Product code (dental resins typically code as “EBF” for tooth shade resin materials)
- Locate the 510(k) summary document, which includes:
- Intended use statement
- Predicate device information
- Biocompatibility testing summary
- Regulatory decision (clearance date and K-number)
What to Look For:
- Clearance Letter: Official FDA document granting 510(k) clearance with specific decision date
- Intended Use Match: Verify the clearance covers your intended clinical application. A resin cleared for models is not approved for aligners.
- Biocompatibility Testing Summary: Confirms ISO 10993 tests completed (cytotoxicity, sensitization, irritation, systemic toxicity, genotoxicity)
- K-Number: FDA’s tracking number for the submission (e.g., K220123)
Cross-Reference with Manufacturer:
Request the 510(k) clearance letter and biocompatibility testing summary directly from the resin manufacturer. Reputable manufacturers provide these documents upon request as evidence of regulatory compliance.
Q13: What should I look for in a resin manufacturer’s biocompatibility documentation?
A: When evaluating resin biocompatibility claims, request and review the following documentation:
- ISO 10993 Biocompatibility Test Report Summary
- Cytotoxicity Testing (ISO 10993-5): Confirm testing was performed using appropriate solvents (aqueous, alcohol, or relevant physiological media) with recognized cell culture methods
- Sensitization & Irritation (ISO 10993-10): Verify testing confirmed no delayed-type allergic response or acute irritation upon mucosal contact
- Systemic Toxicity (ISO 10993-11): Confirm acute toxicity data; for long-term contact devices, subchronic toxicity testing should be included
- Genotoxicity (ISO 10993-3): Verify testing confirmed no mutations or chromosomal damage through Ames test and mammalian cell assays
Red Flag: If biocompatibility claims lack specific ISO 10993 test data, question the manufacturer about testing performed.
- Post-Processing Protocol Validation
- Request documentation showing biocompatibility testing was performed on processed material—after manufacturer-recommended washing and curing
- Verify the cleaning protocol (IPA washing duration, ultrasonic agitation, temperature) is clearly specified
- Confirm UV curing parameters (wavelength, duration, intensity) are validated
Red Flag: Testing performed only on freshly prepared material may not reflect clinical reality if post-processing protocols differ.
- Manufacturing Quality Certificates
- ISO 13485 Certification: Confirms the manufacturer operates a certified quality management system
- FDA Registration: Manufacturer should be registered with FDA as a medical device manufacturer
- Clean Room Certification: For Class II materials, evidence of ISO Class 8 or better clean room manufacturing demonstrates quality control
Red Flag: Manufacturers lacking ISO 13485 or FDA registration may not maintain consistent quality.
- Batch Traceability Documentation
- Each resin batch should be assigned a unique batch number with manufacturing date and expiration
- Manufacturers should maintain records linking each batch to specific biocompatibility and mechanical property testing
- Certificate of Analysis should accompany each batch, confirming testing performed
Q14: What post-processing protocol should I follow to ensure biocompatibility compliance?
A: Manufacturers’ post-processing protocols are validated as part of FDA 510(k) submissions. Deviation from these protocols can compromise regulatory compliance and clinical safety. Here’s a best-practice framework:
Standardized Washing Protocol (Example from LuxCreo DCA Workflow):
- Equipment: Ultrasonic bath with isopropyl alcohol (IPA) solution
- Temperature: Room temperature (23–26°C)
- Duration: Two 8-minute cycles (16 minutes total ultrasonic agitation)
- Equipment Cleaning: Between cycles, manually agitate parts or use dedicated ultrasonic baskets to ensure thorough monomer removal
- Drying: Air dry completely before curing (typically 5–10 minutes at room temperature)
Biocompatibility Rationale: Extended ultrasonic agitation in IPA effectively removes residual uncrosslinked monomers that could leach into saliva. Research demonstrates that extended washing significantly reduces cytotoxicity profiles.
Thermal Curing (if required):
- Equipment: Validated curing oven or heat source
- Temperature: Per manufacturer specification (typically 60–100°C)
- Duration: Per manufacturer specification (typically 10–15 minutes)
- Monitoring: Verify oven temperature with calibrated thermometer; temperature consistency ensures consistent monomer crosslinking
UV Curing:
- Equipment: 405 nm UV curing box or integrated cure station
- Wavelength: 405 nm (specified by resin manufacturer; different materials require different wavelengths)
- Duration: Per manufacturer specification (typically 10–15 minutes per side for aligners/trays)
- Intensity: Confirm curing station intensity meets manufacturer specifications
Quality Control Checkpoints:
✓ Log post-processing times and temperatures for each batch (audit trail)
✓ Verify resin batch numbers match cured part serial numbers (traceability)
✓ Confirm post-cured parts are transparent/clear (visual indicator of proper curing)
✓ Store cured appliances per manufacturer guidance (typically room temperature, protected from UV light)
Documentation: Maintain records documenting your facility’s adherence to manufacturer-validated post-processing protocols. This documentation demonstrates regulatory compliance and provides evidence if adverse events occur.
Risk and Compliance Questions
Q15: What happens if a patient has an adverse reaction to a dental resin I’m using—what are my liability and regulatory obligations?
A: Adverse events involving medical devices trigger specific regulatory and clinical obligations. Understanding these is critical for patient safety and legal protection:
Immediate Patient Care:
- Discontinue use immediately if you suspect the resin caused the adverse reaction
- Document the reaction: Date, symptoms, location, duration, interventions provided
- Provide appropriate clinical management: Treat irritation, sensitization, or allergic responses according to clinical protocols
- Evaluate alternative materials: Consider whether a different FDA-cleared resin would be clinically appropriate
FDA Reporting Obligations (within 30 days):
- If an adverse event occurs (serious injury, death, or malfunction), practitioners are obligated to report to the FDA MedWatch program
- MedWatch submission includes: device information, patient demographics, adverse event description, and outcome
- Portal: https://www.fda.gov/medwatch
Manufacturer Notification:
- Notify the resin manufacturer immediately of any adverse event
- Manufacturers have their own FDA reporting obligations and should investigate root causes
- Request investigation data from manufacturer to assess whether the adverse event was material-related or procedural
Documentation and Legal Considerations:
- Maintain detailed records of the adverse event, patient symptoms, and clinical management provided
- Document when the event was reported to FDA and the manufacturer
- Preserve the resin batch number, post-processing records, and any unused resin from the affected batch
- Consult with professional liability insurance and legal counsel regarding reporting and documentation requirements
Prevention Best Practices:
- Use only FDA-cleared resins with appropriate clearance for your intended clinical application
- Follow manufacturer post-processing protocols precisely; documented adherence demonstrates regulatory compliance
- Obtain informed consent from patients explaining the material, biocompatibility status, and known risks
- Implement quality control procedures catching issues before patient delivery
Regulatory Protection: Using FDA-cleared materials with proper documentation of protocol adherence substantially reduces liability exposure compared to using non-cleared or improperly processed materials.
Q16: Are there any resins I should avoid, and how do I identify potentially problematic materials?
A: While many resins claim biocompatibility, certain characteristics indicate elevated risk. Here’s how to identify potentially problematic materials:
Red Flags for Material Selection:
❌ No FDA Clearance for Intraoral Applications
- Material marketed as “biocompatible” without specific FDA 510(k) clearance for your intended use
- Example: A resin cleared for surgical guides (Class I, external use) inappropriately used for aligners (Class II, long-term mucosal contact)
- Risk Level: High—using non-cleared devices for intraoral applications violates FDA regulations and creates liability
❌ Limited or Absent ISO 10993 Testing Documentation
- Manufacturer cannot provide ISO 10993-5 (cytotoxicity) or ISO 10993-10 (sensitization) test reports
- Testing only performed on fresh material, not post-processed material (which differs significantly in biocompatibility)
- Risk Level: High—indicates inadequate biocompatibility validation
❌ No ISO 13485 Quality Management Certification
- Manufacturer lacks certified quality system; manufacturing processes not validated
- Batch-to-batch variation likely; no traceability between batches and biocompatibility testing
- Risk Level: Medium-High—quality consistency cannot be assured
❌ Open-System Resins Without Validation
- General-purpose 3D printing resins (not specifically formulated for dental/medical use) repurposed for dental applications
- Manufacturers may claim biocompatibility without specific dental validation
- Example: Dental professionals using consumer-grade resin from non-dental 3D printer manufacturers
- Risk Level: Very High—these materials have NOT undergone FDA review for dental applications
❌ Manufacturer Claims Without Substantiation
- Marketing claims like “medical-grade” or “biocompatible” without reference to specific ISO 10993 testing or FDA clearance
- Risk Level: Medium—unsubstantiated claims indicate insufficient regulatory grounding
❌ Resins from Manufacturers with Poor Compliance History
- Manufacturers with FDA warning letters, product recalls, or regulatory enforcement actions
- Check FDA enforcement history: https://www.fda.gov/medical-devices/medical-device-enforcement
- Risk Level: High—past non-compliance indicates ongoing quality or safety concerns
Acceptable Material Characteristics (Green Lights):
✅ FDA 510(k) clearance for your specific intended use
✅ Complete ISO 10993 biocompatibility testing documentation (including post-processed material)
✅ ISO 13485 quality management certification
✅ Manufacturer FDA registration
✅ Clear post-processing protocols with validation evidence
✅ Batch traceability with certificates of analysis
✅ Clinical data demonstrating safety and efficacy
Reputable FDA-Cleared Examples:
- LuxCreo DCA (aligners)
- Formlabs Premium Teeth Resin (restorations)
- 3D Systems NextDent (dentures)
- Desktop Health Flexcera (multi-application)
- SprintRay Ceramic Crown C2 (crowns)
Conclusion
Key Takeaways:
- “Biocompatible” ≠ “FDA-cleared.” Biocompatibility claims without specific FDA 510(k) clearance do not constitute regulatory validation for patient contact applications.
- FDA Class I vs. Class II reflects intended use. Class II intraoral materials (aligners, dentures, splints) require 510(k) clearance; Class I external materials (surgical guides, models) may not.
- ISO 10993 is the comprehensive biocompatibility framework. The FDA and international regulators require specific testing protocols addressing cytotoxicity, sensitization, systemic toxicity, and genotoxicity for long-term contact devices.
- Post-processing protocols directly impact biocompatibility. Manufacturer-validated washing and curing procedures are essential for removing residual monomers; deviations compromise regulatory compliance.
- Select FDA-cleared materials with documented biocompatibility evidence. LuxCreo, Formlabs, 3D Systems, Desktop Health, and SprintRay exemplify manufacturers with comprehensive regulatory validation and clinical evidence.
- International regulations differ by region. FDA 510(k) (USA), CE MDR (EU), PMDA (Japan), and NMPA (China) require separate submissions with distinct evidence packages.
- Documentation demonstrates compliance. Maintaining records of resin batch numbers, post-processing protocols, and biocompatibility certifications provides regulatory evidence and liability protection.
For regulatory affairs specialists, quality assurance teams, and orthodontists concerned with patient safety, selecting FDA-cleared Dental 3D Printing Resins with comprehensive ISO 10993 biocompatibility validation and adhering rigorously to manufacturer post-processing protocols represents the gold standard for ensuring clinical safety and regulatory compliance.
Subscribe to Our Newsletter
Be the first to get our latest updates and free trials!
Popular Resources
Follow Us
Featured Products

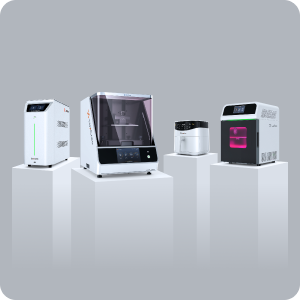
4D Aligner™
First Smart ActiveMemory™
Aligner

iLux Pro Dental Solution
Ultimate 1-Click Dental
Application Solution

LuxCloud Dental
Your One-stop Digital Dentistry
Platform